Let’s Dig Into Everything about RA
Navigate:
- What is Rheumatoid Arthritis?
- The causes of RA
- Rheumatoid Arthritis symptoms
- Diagnosing RA
- Rheumatoid Arthritis (RA) vs. Osteoarthritis (OA)
- Next steps
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes pain, swelling, stiffness, and loss of function in the joints.
A healthy immune system protects the body by attacking foreign organisms such as bacteria and viruses. However, in cases where an autoimmune disease exists, the body mistakenly attacks healthy tissue instead. In RA, the joints which are designed to absorb shock and allow smooth movement between bones, are targeted by the autoimmune process.
About 1.5 million people in the United States have rheumatoid arthritis.
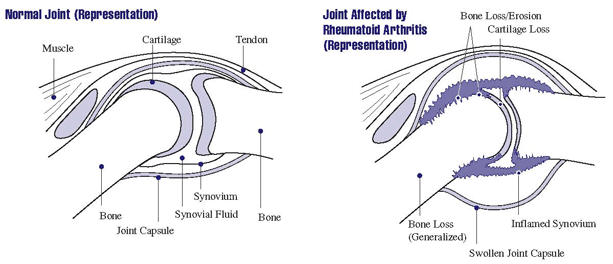
The ends of your bones are covered by elastic tissue called cartilage, which supports and helps protect the joints during movements. A tissue known as synovium or synovial membrane lies next to the cartilage. The synovium produces synovial fluid, a substance that acts as a lubricant and provides nourishment to the cartilage.
In people with RA, the autoimmune process causes the synovium in certain joints to become inflamed. The tissue swells and becomes painful with every movement of the affected joints.
The uncontrollable joint inflammation can also lead to joint erosion, a loss of motion, and joint damage to many associated parts of the body. In other words, people with rheumatoid arthritis will likely experience worsening pain and stiffness, especially if this particular inflammatory arthritis isn’t treated with non-steroidal anti-inflammatory medications or other standard treatment protocol.
RA affects the most important joints in the body, including joints in the:
- Hands
- Feet
- Wrists
- Elbows
- Knees
- Ankles
Over time, the affected synovium along with the cartilage and bone next to it become eroded. Everything around the synovium meant to support the joint — muscles, ligaments, and tendons – slowly weaken. This breakdown, along with friction caused by a less functional synovial fluid leads to most of the pain commonly associated with RA.
The Best Rheumatoid Arthritis Treatment Begins Early
It is important to diagnose and begin treatment for rheumatoid arthritis early, as permanent damage to bones can begin within the first year of developing the disease.
For this reason, it is necessary to realize that RA often begins in middle age and nearly 3 times as many women have the condition as men. And, although it does not usually occur in children and young adults, a related disease called juvenile idiopathic arthritis (JRA) or juvenile rheumatoid arthritis (JRA) can sometimes develop.
Overall, RA is a slowly progressing disease, but once the damage is done it cannot be reversed. Therefore, doctors recommend treatment of rheumatoid arthritis beginning immediately after diagnosis to slow down the effects.
Causes of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disorder, meaning it is caused by an anomaly in the immune system. However, doctors are not sure what causes the immune system to attack its own tissues. That being said, they have identified what likely contributes to the disease.
Genetic Factors
Certain genes may play a role in the development of RA. Since the 1970s research has shown that people with certain genetic markers are more susceptible to developing rheumatoid arthritis. The human leukocyte antigen (HLA) known as more specifically as “HLA-DRB1” was identified as a gene locus – a region or collection of genes, that is associated with RA.
Even though studies have suggested that people who have these genes could be many times more likely to develop RA than people without it, you should note that not everyone with RA has the linked HLA genes. Additionally, not everyone with the HLA gene will develop RA. These genes do not cause RA, instead they make certain patients more likely to develop it.
Environmental Factors
There are several environmental and occupational factors that, when combined with a genetic predisposition, put people at a greater risk of developing RA. Some of these factors include:
- Certain bacteria and viruses
- Exposure to second-hand smoke
- Air pollution and exposure to certain chemicals and mineral oils
- Silica mineral (found in obsidian, granite, diorite, and sandstone)
Personal Factors
Gender: Both men and women are susceptible to RA, but the disease is far more common in women. In fact, 70 percent of people diagnosed with rheumatoid arthritis are women. This may be due to a variety of factors that are involved in the development of RA. For instance, changes (such as those caused by the use of certain contraceptives) have been linked to promoting the development of RA in people who are genetically susceptible or have been exposed to a triggering event. Rheumatoid arthritis symptoms also tend to improve or disappear completely during pregnancy, with frequent flares more common after the birth. Breastfeeding can also cause RA symptoms like joint inflammation and low-grade fever to flare.
Age: RA can affect a person at any age, but it typically presents in those between the ages of 40-60. Some cases of juvenile rheumatoid arthritis do exist though, so it’s important to be aware of this in the event that a minor starts experiencing RA-related symptoms. Remember: early detection is the key to successful treatment of rheumatic disease.
Family History: People who have a family history of rheumatoid arthritis may have a higher chance of developing the disease themselves.
Research on Rheumatoid Arthritis
In the last decade, much research has been conducted to increase our understanding of the immune system and what makes it malfunction. There have also been new therapies developed to help treat the disease. Some of the topics of intense research include:
What are the genetic factors that predispose people to develop rheumatoid arthritis?
Some white blood cells, commonly known as T cells, are important in maintaining a healthy and properly functioning immune system. However, scientists have discovered a variation—called single nucleotide polymorphism (SNP)—in a gene that controls T cells. When the SNP gene variation is present, T cells attempt to correct abnormalities in joints too quickly, causing the inflammation and tissue damage associated with RA. The discovery of SNP may help determine people’s risk for getting RA and might help explain why autoimmune diseases run in families.
At conception, twins have an identical set of genes. So why would only one twin develop RA?
Twins only have identical genomes at conception. After birth, developmental and environmental factors experienced through the stages of growth differentiate the genomes. By studying the differences in the lives of twins then, scientists can better determine where and why rheumatoid arthritis begins to develop. A technique called microarray is used to examine a large number of genes at once and find differences that may develop in cases such as those involving twins. Thanks to these types of studies, researchers have been able to identify several genes that may be associated with inflammation and bone erosion seen in people with RA.
Rheumatoid Arthritis Symptoms
Rheumatoid arthritis is a joint inflammation disease which begins slowly and progresses over time. Unfortunately, it can sometimes be difficult to detect and diagnose RA because early symptoms are often subtle and nonspecific.
A couple of these early symptoms of the disease include fatigue, stiffness, and tenderness in the joints, which can be symptoms of other, less severe conditions as well. Furthermore, symptoms appear differently in most patients and many may have periods of time where they experience no symptoms at all.
There are many other symptoms of rheumatoid arthritis that stem from inflamed tissue in the joints. Some of the most common symptoms reported by people with rheumatoid arthritis are:
-
-
- Swelling: Synovial tissue in the caps of joints becomes damaged in rheumatoid arthritis sufferers, causing the tissue to thicken and swell.
- Stiffness: Inflamed joints tend to stiffen and are difficult to move correctly. People who have RA experience stiff joints, especially in the mornings or after long periods of rest. This can last for hours at a time.
- Pain: Cartilage and bone within the joints will wear down over time. Joints are supported by surrounding muscles, ligaments and tendons, but, with RA, these will weaken and no longer stabilize joints. This causes intense pain and joint damage as a result.
- Redness: Joints can be warm and may appear pink (or even red) on the outside during a flare or when inflamed.
-
The degeneration caused by RA tends to affect the smaller joints in the body first, namely the joints in the fingers, hands, and feet. The damage then spreads to other major joints in the body.
Heavy inflammation of the joints is known as a flare, and flares are common in RA sufferers, sometimes lasting for months at a time.
Additionally, RA usually affects the body symmetrically, which means the same joints on both sides of the body will show symptoms at the same time. For instance, if one wrist begins showing symptoms, the other will likely show symptoms within the near future.
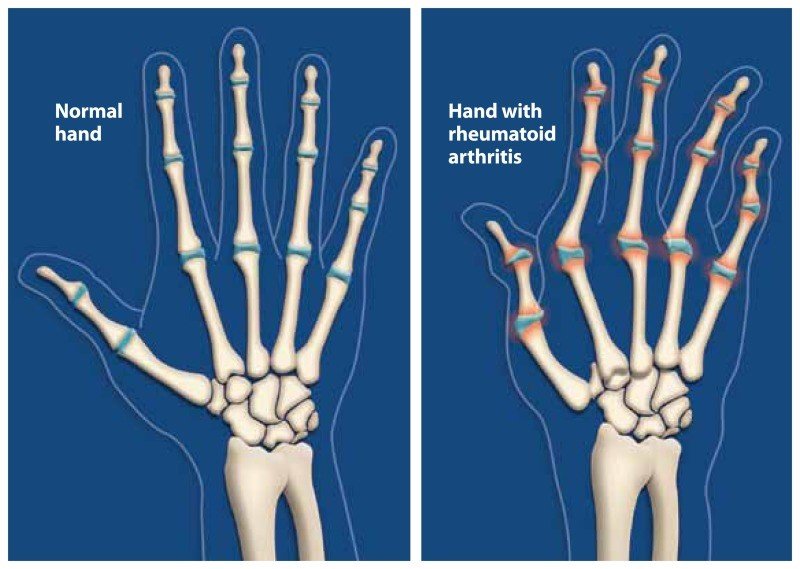
RA is most common in the hands, but can happen in any joint, including knees, wrists, neck, shoulders, elbows, feet, hips, and even the jaw.
Physical Symptoms
Physical symptoms are the direct result of the high levels of inflammation that come with RA. These can affect the entire body and sometimes resemble the flu, but are chronic (or longer lasting) in nature.
Some of the most common physical symptoms include:
- Fatigue
- Minor fever
- Loss of appetite
- Skin rash
- Muscle aches
- Neck pain (if the RA is in the cervical spine)
- Morning stiffness
- Weight loss
There are similar symptoms that appear in specific locations in the body.
- Shortness of breath can come from inflammation and scarring of the lungs. A sharp chest pain frequently appears as well.
- Dry eyes and dry mouth can be signs of Sjögren’s Syndrome, an immune disease that often accompanies rheumatoid arthritis. In Sjögren’s Syndrome, the glands in your eyes and mouth that typically produce mucus and moisture no longer produce effectively.
- Other eye symptoms can include burning, itchiness, discharge and impaired vision.
- Rheumatoid nodules are small lumps that form under the skin over bony areas that have been eroded away. Nodules are firm and are usually non-painful. Fortunately, the frequency of nodules in RA patients dwindles every year because of early detection and symptom control. As a result, currently only approximately 20% of rheumatoid arthritis patients have developed these nodules.
- Inflamed blood vessels from long-standing rheumatoid arthritis can lead to damage in nerves and skin resulting in numbness, tingling, and burning. This is called rheumatoid vasculitis.
- Anemia, the decrease in production of red blood cells, is also a common symptom of rheumatoid arthritis.
Psychological Symptoms
While physical symptoms differ in severity and frequency, sometimes the person with rheumatoid arthritis feels it in other ways. In other words, RA may also cause emotional and psychological symptoms as it affects every person differently.
For example, the symptoms of RA can leave a person unable to function for long periods of time without pain. This means that jobs which involve a large amount of moving around or a large amount of time sitting still can be difficult for a person with RA.
This type of work-based limitation can lead to mental illnesses such as depression, anxiety, low self-esteem, and feelings of helplessness. All of these psychological struggles can be fairly common among RA sufferers.
If you or someone you know is experiencing these symptoms, it’s important to see a doctor as soon as possible. Diagnosing RA early is necessary due to how quickly bone and cartilage damage can occur.
Click here to learn more about rheumatoid arthritis symptoms.
Diagnosing Rheumatoid Arthritis
Rheumatoid arthritis is subtle and often presents itself similarly to other arthritis diseases. Early symptoms include minor joint pain, stiffness, and fatigue, but these are often attributed to other, less problematic causes. For instance, sometimes symptoms will resemble the flu, making RA more difficult to detect.
However, people will typically feel the effects of RA in their smallest joints first, such as the fingers and toes. The earliest signs of the disease are:
- Achy joints
- Stiffness
- Formation of nodules
- Fatigue
- Unintentional weight loss
If a doctor suspects that a patient has RA, they will refer the patient to a rheumatologist for further testing. A rheumatologist is a medical professional who specializes in musculoskeletal and autoimmune diseases and is specially trained to handle the diagnosis and treatment of RA and other arthritis diseases (such as psoriatic arthritis, seronegative rheumatoid arthritis, and Felty syndrome).
Tests performed by a rheumatologist to determine whether RA exists include:
- Family history: A rheumatologist will first ask for the medical history of the patient to see if RA or other arthritis diseases run in their family. Many scientists believe that having a certain gene increases the chances of developing RA, and they also believe that gene can be inherited.
- Pain history and examination of joints: A rheumatologist can get a better understanding of disease progression if he or she knows the patient’s recent and current symptoms. That’s why it is so important to keep an accurate record of pain and other symptoms, to ensure a proper diagnosis is made. Once a rheumatologist understands a patient’s pain history, a physical examination is performed on the joints. The physical examination can tell the rheumatologist the progression of RA and where in the body it is affecting. If RA has started to develop in the joints, a patient will often show signs or sensitivity to tenderness, swelling, warmth, and painful or limited movement.
- Blood tests: Blood chemistry can tell a rheumatologist a lot about inflammation levels, making it a good determinant of rheumatoid arthritis. Put another way, if certain antibodies are present in the blood, there is a high chance that the person has RA. One of these antibodies is known as Rheumatoid factor, or RF. Rheumatoid factor is a protein which attacks healthy tissues. So, if a blood test shows that rheumatoid factor is present, there is an 80% chance the patient could develop RA or another inflammatory disease. Other blood indicators include the erythrocyte sedimentation rate (ESR), tumor necrosis factor-alpha, or c-reactive protein (CRP) levels, as all of these may indicate the presence and level of inflammation in the body.
- Imaging scans: Joint damage can be detected through imaging tests, making these useful tools for diagnosing rheumatoid arthritis. Rheumatologists use x-rays, ultrasounds, and magnetic resonance imaging scans to examine the joints and determine if RA is the cause of erosion. However, damage will not always be present with a positive RA diagnosis if the disease is in an early stage.
No single test can determine if a person has rheumatoid arthritis. Rather, rheumatologists use a combination of tests to make an accurate diagnosis. If a diagnosis is made, the patient will work with a rheumatologist to create a treatment plan that fits his or her needs and current stage of RA.
Click here to learn more about diagnosing rheumatoid arthritis.
The Stages of RA
Rheumatoid arthritis most often develops as a progressive disease, meaning that it will become more aggressive over time. However, this isn’t always the case as it can also appear in other types of progressions as well.
Monocyclic progression (sometimes called remissive) is an episode of RA with symptoms that last only 2-5 years. Monocyclic progression is usually the result of an early diagnosis and immediate aggressive treatment to ensure that the symptoms do not return.
Polycyclic progression (sometimes called intermittent) is the constant recurrence of RA symptoms and flares, but in fluctuating stages. With polycyclic progression, patients can go long periods of time without experiencing any symptoms at all, but flares usually return.
Rheumatoid Arthritis vs. Osteoarthritis
Many people confuse rheumatoid arthritis with osteoarthritis (OA) due to their similar symptoms, but the two diseases are caused by different factors.
What is Osteoarthritis?
Whereas rheumatoid arthritis is an autoimmune disease that causes joint malfunction due to inflammation, osteoarthritis is a mechanical disease brought on by the destruction of joints through wear and tear.
Osteoarthritis is the most common form of arthritis, with approximately 27 million Americans over the age of 25 having been diagnosed with it. Osteoarthritis is also most commonly seen in people middle-aged to elderly and is the top cause of disability in those age groups, though it can also appear in younger people who have sustained joint injuries.
With osteoarthritis, the cartilage, joint lining, ligaments, and bone are all affected by deterioration and inflammation. When the cartilage begins to break down due to stress or changes in the body, the surrounding bones slowly get bigger and begin to fail.
Osteoarthritis is a slowly progressing disease and occurs in the joints of the hand, spine, hips, knees, and toes. Furthermore, risk factors of this disease most often stem from lifestyle or biological causes, such as:
- Obesity
- Old age
- Genetic recurrence or defect
- Overuse of joints
- Job stresses
- Sports injuries
Osteoarthritis sometimes occurs alongside rheumatoid arthritis or other disease, such as gout.
Symptoms of OA
Symptoms of the breakdown of joints and the weakness of bones associated with osteoarthritis include:
- Joint pain and stiffness
- Knobby swelling at the joint site
- Grinding or cracking noises at joint site during movement
- Decreased joint function
While rheumatoid arthritis occurs symmetrically in the body—meaning that when a joint on one side is affected, the joint on the other side will likely be affected as well—osteoarthritis does not occur symmetrically in the body. It affects a single joint or a joint on one side of the body more severely. It also progresses slowly over the years and can worsen with sudden injuries or increased risk factors.
Diagnosing OA
When diagnosing osteoarthritis, a rheumatologist looks for warning signs that coincide with an individual’s risk factors. Physical exams, x-rays, and other imaging tests are used to determine whether a patient has osteoarthritis, as well as to determine the severity of the disease if it exists.
Treating OA
Like rheumatoid arthritis and other similar diseases of the joints, damage from OA cannot be reversed. However, there are treatment options and lifestyle changes that can reduce pain and improve the function of the affected joints:
-
- Lifestyle Changes: Being overweight is a large risk factor for osteoarthritis because it puts a large amount of stress on weight-bearing joints. This damage is largely preventable by losing excess weight and increasing safe activity. Exercise (as long as it does not put dangerous strain on the joints) can improve your muscle strength and strong muscles will better support your weight-bearing joints, ultimately lowering the chances of developing the negative symptoms of OA. Getting a sufficient amount of rest is also necessary for management of OA symptoms.
- Non-Drug Therapies: Some patients find that sore and painful joints can be soothed by holistic alternatives to drugs. Massages, chiropractic manipulation, spa visits, and acupuncture are options which are said to relieve pain, but generally only for short periods of time, or until the treatment procedure is repeated.
- Natural Home Remedies: Many sufferers have found significant pain and inflammation relief and sometimes complete remission with lab grade turmeric and boswellia combinations. These seem to be especially effective when combined with an autoimmune diet.
Drug Therapies:
Osteoarthritis is treated with many of the same medications as rheumatoid arthritis. Nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease swelling and pain are often the first method of treatments. Other options include oral pain relievers such as acetaminophen and topical drugs such as capsaicin cream, lidocaine, and diclofenac gel. These drugs are typically over-the-counter, but stronger prescription medication can be prescribed by a doctor if necessary.
Prescription drugs include:
- Corticosteroids (or cortisone shots), which are often used to provide temporary relief of OA. For instance, these shots, administered directly into the knee, can delay the need for knee surgery, largely because of the relief they provide.
- Cymbalta, which is typically a drug used to treat depression, was approved by the FDA to treat chronic musculoskeletal pain, like that associated with OA.
Click here to learn more about the differences between RA and OA.
Next steps
If you or someone you care about is experiencing symptoms consistent with those associated with rheumatoid arthritis, it’s important to make an appointment with a doctor as soon as possible. The earlier RA is diagnosed, the earlier treatment can be started to minimize the long-term damage to the joints.
There are many effective medications and RA treatment options available, all of which can provide hope after a diagnosis. Some include working with a physical therapist, others involve platelet-rich plasma therapy, and still others mean something as simple as taking daily DMARDs.
DMARD is an acronym for disease-modifying antirheumatic drugs and these are medications designed to help protect the health of the joint by essentially blocking the inflammation from seeping in. Some of the most common DMARDs include Azathioprine, Leflunomide, and Methotrexate. However, there are a number of different antirheumatic drugs, medications, and other anti-inflammatory agents available for treating rheumatoid arthritis.
If you would like to know more about the various medications and treatment options available for RA, click here.
For helpful tips and advice about living with RA, click here.
