PsA: What is Psoriatic Arthritis?
Have you ever heard of psoriasis? Most likely yes. Either you or someone you know suffers from red, patchy, itchy skin, with silvery scales. A fairly common autoimmune disorder, psoriasis affects approximately 7 million individuals in the United States alone. What you may be less familiar with is arthritis that affects psoriasis sufferers. Termed psoriatic arthritis, this autoimmune disorder affects 30% of individuals who have psoriasis.
Psoriatic Arthritis Facts and Statistics
Psoriatic arthritis is an autoimmune disorder, what this means is that the body is turning on itself, essentially attacking the tissue that makes up its own joints. While psoriatic arthritis can develop at any time, the most likely age of onset is between 30 and 50, with most cases presenting first signs between the fourth and fifth decade. Chronic and progressive, psoriatic arthritis affects men and women equally. The detailed epidemiology of psoriatic arthritis is as yet unclear due to the lack of universally accepted criteria for the diagnosis of the disease. About 85% of people diagnosed with psoriasis will go on to develop psoriatic arthritis at some point in the course of the disease, and a small percentage of individuals will develop psoriatic arthritis without suffering from psoriasis.
Medical scientists still have not pinpointed an exact cause of psoriatic arthritis; however, most doctors have come to agreement that it is a mix of genetics and the environment that plays a role in who develops this condition. The strongest predictor of whether someone develops psoriatic arthritis is if they are already suffering from psoriasis. The second predictor of psoriatic arthritis is having a family history of psoriasis or psoriatic arthritis. Environmental factors, such as stress certain bacterial or viral infections (e.g., strep throat) are also believed to play a role in the onset of psoriatic arthritis.
Types of Psoriatic Arthritis
The three most common types of arthritis, osteoarthritis, rheumatoid arthritis, and psoriatic arthritis, have many overlapping symptoms, sometimes making the diagnosis of psoriatic arthritis difficult. In many cases, the presence of psoriasis is the determining and distinguishing factor that helps a physician to make the diagnosis of psoriatic arthritis.
Once a psoriatic arthritis diagnosis has been made, your doctor will likely classify you into one of five types of psoriatic arthritis. We discuss these types below.
- Symmetric psoriatic arthritis
- Asymmetric psoriatic arthritis
- Distal psoriatic arthritis
- Spondylitis
- Arthritis mutilans
Symmetric psoriatic arthritis
In this form of psoriatic arthritis, joints on both sides of the body are affected. The most common type of psoriatic arthritis is symmetric psoriatic arthritis. It affects about 50% of the psoriatic arthritis population. Symptoms of symmetric psoriatic arthritis are similar to rheumatoid arthritis symptoms.
Asymmetric psoriatic arthritis
Affecting approximately 35% of the population with psoriatic arthritis, asymmetric psoriatic arthritis appears in different joints on different sides of the body. Instead of both knees being inflamed, your knee might be affected by psoriatic arthritis on the right side of your body and your left elbow might be inflicted with pain and inflammation at the same time.
Distal psoriatic arthritis
Distal psoriatic arthritis affects the fingers and toes. Some characteristics of this type of psoriatic arthritis are swollen, inflamed joints and nail changes – including nail pitting, white spots within the nails, and nails lifting from the nail bed.
Spondylitis
Spondylitis is a type of psoriatic arthritis that primarily affects the back and the spine. Painful swelling and inflammation in these areas are classic symptoms of spondylitis.
Arthritis mutilans
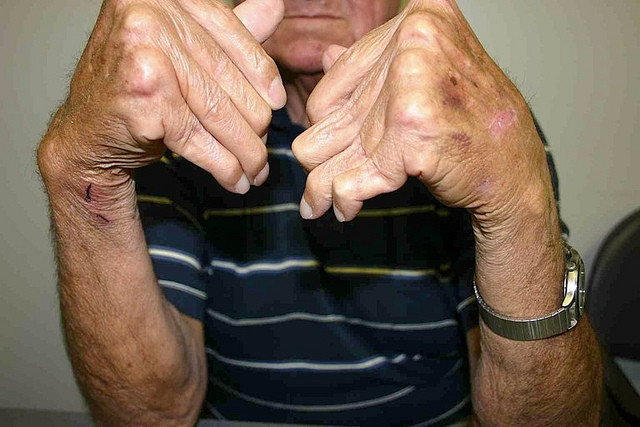
Arthritis mutilans only affects a very small percentage of psoriatic arthritis sufferers (approximately 5% of the population) and it is the most severe type. Arthritis mutilans causes intense joint inflammation leading to permanent deformities in the fingers and toes, destroying the joints so severely that full recovery is often not attainable.
Symptoms of Psoriatic Arthritis
If you suspect you or a loved one is affected by psoriatic arthritis, what are the signs and symptoms you should be looking for? Below is a list of some of the most common symptoms of psoriatic arthritis. You might have only a couple of the symptoms on this list or you might have several.

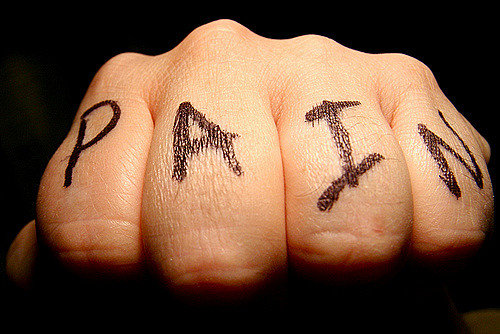
- Joint pain
- Inflammation
- Stiff joints – especially after sleeping or resting for long periods of time
- Generalized fatigue
- Swelling and pain in the tendons
- Swollen fingers and toes (“sausage-like” appearance termed dactylitis)
- Reduced range of motion
- Nail pitting or any other type of nail changes that look similar to nail fungus
- Eye pain and redness – mimicking signs of conjunctivitis (i.e., pinkeye)
- Lower back pain
- Heel pain

If you are experiencing any of the above symptoms and suspect you might be suffering from psoriatic arthritis, contact your physician. Your doctor will conduct a general medical exam, ask you a number of questions about your symptoms and family history, and will also include some blood work.
Because psoriatic arthritis has many overlapping symptoms with osteoarthritis, rheumatoid arthritis, and gout, your doctor may run some tests to rule out these other types of arthritic conditions. For example, you might undergo Rheumatoid factor (RF) and anti-CCP antibody tests to rule out related rheumatoid arthritis, x-rays to examine joint damage and inflammation, and bone density scans to measure your bone health. While the exact cause of psoriatic arthritis is unknown, many individuals with psoriatic arthritis (approximately 40-50%) have the HLA-B27 genotype. A simple blood test can confirm this genotype in the body and help with the diagnosis.
Treatment Options
If you have been diagnosed with psoriatic arthritis, what are your treatment options? Thankfully, treatment options for arthritis have advanced in recent years and many individuals living with psoriatic arthritis keep symptoms and pain under control by following a regimen of treatments.
Treatments for psoriatic arthritis can include medication, surgery, and lifestyle changes.

The most common medications for psoriatic arthritis treat the most prominent symptom of the disease: inflammation. The following are several common medications used in the treatment of psoriatic arthritis.
- NSAIDs: Non-steroidal anti-inflammatory drugs are some of the most commonly prescribed prescription medication options for treating psoriatic arthritis. NSAIDs give pain relief and inflammation reduction. Rare side effects of this type of drug include stomach irritation, liver and kidney damage, and heart problems.
- DMARDs: Disease-modifying anti-rheumatic drugs can slow joint damage. Rare side effects include lung infections, bone marrow suppression, and liver damage.
- Immunosuppressants: Immunosuppressants are designed to calm the immune system, which is a significant need with an autoimmune disorder, such as psoriatic arthritis. Autoimmune disorders turn on the body and attack healthy systems, so this type of drug can block those type of responses. Potential side effects are significant and include an increased susceptibility to infections.
- TNF-alpha inhibitors: This type of medication treats joint inflammation and reduces pain, stiffness, and swollen joints. Potential side effects can include upset stomach and hair loss.
Some individuals with psoriatic arthritis take steroid injections to quickly reduce inflammation into affected joints. Joint replacement surgery may be necessary for some individuals with the disease to replace severely damaged joints with artificial prostheses.
Lifestyle changes can have profound effects on the management of psoriatic arthritis symptoms. Maintaining a healthy lifestyle can make a world of difference in the pain and inflammation associated with this disease. Some common lifestyle changes include:
- Protecting the joints: Taking care to approach common everyday tasks in “joint-saving” manners can make a world of difference in the pain associated with psoriatic arthritis. Examples include simple life changes such as opening a jar lid with a jar opener (instead of putting the strain on your fingers and wrist), lifting objects with both hands, and pushing open doors with your body weight instead of your fingers.
- Exercising regularly: Exercising regularly can increase your range of motion and reduce the stiffness of the joints. Good exercises for individuals with psoriatic arthritis include biking, swimming, and walking.
- Keeping a healthy weight: Excess weight causes trauma and stress to the joints. Maintaining a healthy weight will reduce the increased stress to your body and lessen symptoms of psoriatic arthritis.
- Taking it easy: Psoriatic arthritis can cause great fatigue. Taking rest breaks often or splitting your work up into multiple segments can help you manage this fatigue
Prognosis and Prevention
Can psoriatic arthritis be prevented? Unfortunately, no. However, with proper treatment, the prognosis for people living with psoriatic arthritis is good. As soon as you start to exhibit symptoms, it’s best to get checked out by a doctor, as the sooner you start treatment, the better the prognosis becomes. You don’t want to wait until so much damage is done to the joints they aren’t treatable or are only treatable by more extreme means (e.g., surgery).

When diagnosed with psoriatic arthritis, there are dietary changes that may potentially help prevent a flare-up of the condition. Your physician will educate you on which portions of your diet may assist in the treatment. As mentioned above, maintaining a healthy weight and cutting down on “empty” calories such as sodas, sugars, candy, and other junk food, can keep extra pressure off of the joints. Psoriatic arthritis patients have also reported when they eliminate or diminish dairy products from their diet, symptoms are lessened.
When you have a psoriatic arthritis flare-up, pay attention to changes in your diet or lifestyle that could have contributed to the flare-up. Do you consume a lot of dairy or were you particularly stressed out about work or life in general? If you spot the triggers of psoriatic arthritis flare-ups, you can learn to minimize the introduction of those triggers in your everyday life.
Once you have a good handle on your treatment options and daily lifestyle changes, living with psoriatic arthritis can be manageable and relatively pain-free. Know the symptoms, pay attention to the triggers, and be proactive with your health.
